We include products in articles we think are useful for our readers. If you buy products or services through links on our website, we may earn a small commission.
Insulin Resistance Diet: Separating Fact From Fiction

Table of Contents
An insulin resistance diet is a way of eating to prevent and even reverse diabetes, obesity, high blood pressure, PCOS, and other chronic metabolic disorders.
This approach to treating metabolic disorders with a diet targeting insulin resistance is based on:
- research showing that insulin resistance is the link underlying these many different disorders.1
- research showing that dietary changes can dramatically improve insulin resistance.2
In this article, we’ll explore what insulin resistance is, how an insulin resistance diet can control it, and what dietary approaches work best according to available research.
What is Insulin?
Insulin is a hormone produced by the pancreas. Its purpose is to regulate blood sugar by triggering your cells to accept and use blood sugar (glucose) as fuel.
What is Insulin Resistance?
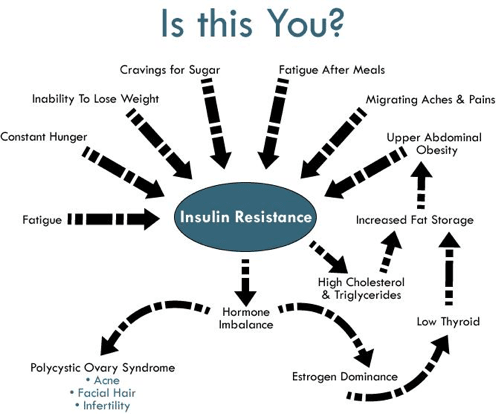
Insulin resistance is a condition that occurs when cells become “resistant” to the chemical signaling of insulin telling them to accept glucose.
This process results in keeping blood sugar levels toxically high resulting in a cascade of metabolic and hormonal disorders.
Insulin resistance entails a metabolic cycle where:
- Large amounts of glucose enter and remain in the bloodstream
- Your pancreas releases high levels of insulin to try and force this excess blood sugar into cells
- Your cells increase their resistance to insulin and require greater amounts of insulin to allow sugar in[2]
- Insulin producing cells in your pancreas get burned out, limiting your ability to make insulin in the future
- Blood sugar remains chronically high leading to obesity, diabetes, fatty-liver disease, high blood pressure and other disorders
What Causes Insulin Resistance?
When you eat carbohydrates including added sugars, whole grains, vegetables, and fruit, your body breaks them all down into simple sugars (glucose) that gets sent into your bloodstream.
When you eat a chronically high amount of carbs, like most people on a Standard American Diet, your body is forced to produce chronically high levels of insulin. This sets off the cycle outlined above.
Insulin resistance is caused by our calorie-dense, carbohydrate-dominant diets, combined with lack of activity. In other words, we eat too much processed, sugary junk food, and don’t move enough.
How Can Diet Prevent and Reverse Insulin Resistance?
For decades the mainstream protocol for an insulin resistant diet has called for:
- Consuming fiber-rich whole grains, fruits, and veggies
- Cutting fat
Why Fiber?
This protocol is centered on the idea that fiber slows down the digestion of carbohydrates into glucose (blood sugar), protecting against glycemic (blood sugar) spikes. Reducing glycemic spikes, in turn, reduces insulin spikes.
Why Cut Fat?
The embargo on fat has to do with the fact that 1 gram of fat provides twice as many calories as 1 gram of protein or carbs.
Since most people with metabolic syndrome are obese, nutritionists see a need to reduce overall caloric intake.2
However, as we mentioned above, grains, veggies, and fruits all get broken down into simple sugars that require insulin.
This begs the question: Is a high-carb diet actually effective against insulin resistance? And are there better low-carb options?
Interestingly, a 2005 study set out to explore this question, which we’ll look at in more detail next.
High-fat Low-Carb vs. Low-Fat High-Carb
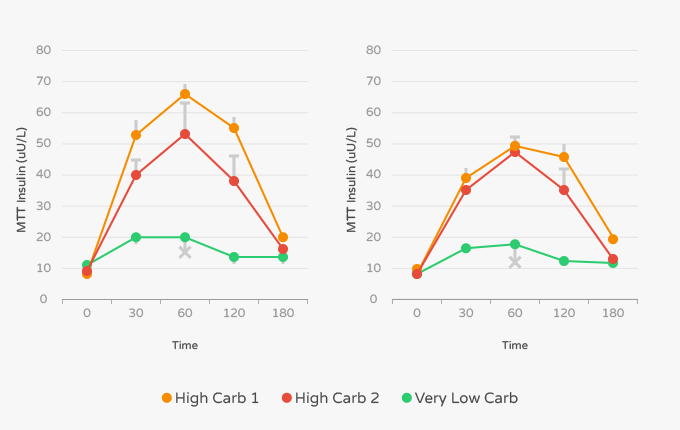
In 2004 researchers set out to determine the effects that 3 different popular diets had on insulin resistance.
They compared the standard insulin diet of high-carb, high-fiber, low-fat, against both a low-carb high-fat “Aitkins” diet, and a low-carb high-protein “Zone” diet. The study followed 96 obese and insulin-resistant women for 8 weeks.
Researchers found that “reduction to body weight, waist circumference, triglycerides, and insulin levels decreased with all three diets, but, reductions were significantly greater in the high-fat and high-protein groups than in the high-carb group.”3
They concluded, “These observations suggest that the popular diets reduced insulin resistance to a greater extent than the standard dietary advice did.”
In 2006 researchers conducted a similar study 2006, dividing 83 obese participants into three groups eating calorically equal portions: Group 1 ate a very low fat det (VLF) where 70% of calories came from carbs, 10% fat (3% saturated fat), and 20% protein.
The group two diet was high in unsaturated fat (HUF), with 50% carbs, 30% fat (6% saturated fat), 20% protein. Group 3 ate a ketogenic diet, or what researchers called “very low carbohydrate diet” (VLCARB) that wasf 4% carbohydrates, 61% fats (20% saturated fat), and 35% protein.
After 8 weeks each diet showed similar reductions in body weight and fat loss. The VLCARB diet, however, lowered fasting insulin by 33%. While the HUF diet lowered insulin by 19%. [6] Not surprisingly, the VLF diet showed zero impact on insulin levels.
According to the researchers, “the VLCARB meal also provoked significantly lower postprandial glucose and insulin responses than the VLF and HUF meals.” [6]
In addition to the effects on insulin the VLCARB diet also reduced triglycerides more than the other diets. Researchers concluded that “VLCARB may be useful in the short-term management of subjects with insulin resistance and hypertriacylglycerolemia.”2
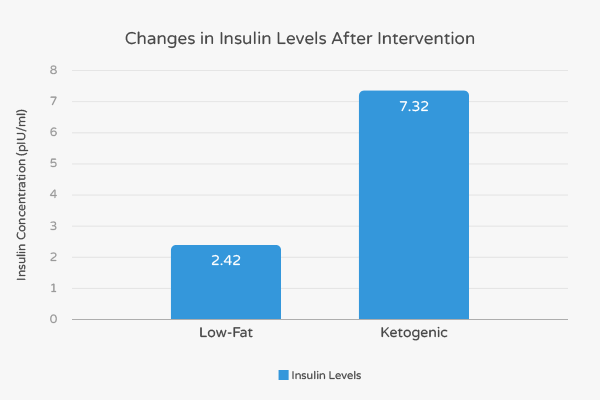
A 2010 study looking at a diverse population of 146 overweight and obese subjects compared a ketogenic diet with a low-fat diet supplemented with weight-loss medication.
Researchers found that insulin levels for the subjects on the ketogenic diet decreased 300% more than subjects on the low-fat drug-assisted diet. 8
Mediterranean Keto for Insulin Resistance
The Mediterranian keto diet takes the keto-friendly foods found in a traditional Mediterranean diet and formulates them into an eating plan that meets the keto macronutrient ratios of 70-80% fat, 15-20% protein and 0-10% carbs.
A typical Mediterranean keto consists of:
- Fish and seafood as the primary source of protein and animal fat
- Olive oil as the primary source of added fat
- Green vegetables and salads as the main source of carbohydrate
- 1-2 cups (200-400ml) of red wine per day
A 2011 pilot study was conducted to look at the effects of what researchers called the Spanish Keto Mediterranean Diet (SKMD) on 22 obese men.[19] All 22 participants had metabolic syndrome.
After 12 weeks the study found that:
- Fasting blood sugar levels dropped from a pre-diabetic 118 to an ideal 91
- Subjects lost an average of at least 30 pounds
- All participants no longer had metabolic syndrome
- They lost an average of 6 inches (16 centimeters) from their waist
- Body mass index (BMI) dropped from 37 to 31.5: This represents a change from class 2 obesity to the low end of class 1.
- An increase in “good” HDL cholesterol from 44 to 58.
- A decrease in triglycerides from 224 to 109
- A change from “prehypertensive” to “normotensive”
- Markers for fatty liver disease including liver enzymes and liver fat reduced, and in some cases completely resolved [21]
It’s interesting to note that though most participants completed the study still on the lower scale of obesity, their metabolic syndrome was completely reversed.
This suggests that losing weight isn’t the main factor in curing metabolic disease. Rather, the power of these changes is attributable to the diet itself.
The takeaway: An Mediterannean keto way of eating is likely an effective insulin resistance diet.
Intermittent Fasting for Insulin Resistance
Another element you may want to consider adding to your insulin resistance diet is the practice of intermittent fasting.
Intermittent fasting entails alternating between designated periods of eating and not eating throughout the day or week.
There are numerous intermittent fasting strategies to choose from, like the popular 16/8 method, the OMAD diet, and the gentler circadian rhythm fasting plan. There are even intermittent fasting strategies for women, whose bodies are more sensitive to calorie restriction.
A 2018 study showed that therapeutic fasting can reverse insulin resistance. In the study, patients were able to wean off insulin therapy without altering their blood sugar levels. At the same time, they shed significant body weight and reduced waist circumference.3
Another study looking at intermittent fasting vs. overall calorie restriction for the treatment of type 2 diabetes found that intermittent fasting showed a 3-6% reduction in blood sugar, and lowered insulin an average of 20-31%. 4
In addition, there is research suggesting that combining intermittent fasting and keto can mutually enhance the benefits of each approach.
The takeaway: Intermittent fasting can be a powerful addition to your insulin resistance diet.
Why High-Fat Low-Carb Diets Improve Insulin Sensitivity
High-fat, low-carb diets like keto and carnivore target insulin resistance in three key ways:
- They reduce carbs
- Offer more nutrient-dense foods
- Fuel the body with ketones
By cutting carbs you are dramatically reducing your primary source of blood sugar. Less blood sugar means less need for insulin. Your cells then re-sensitize to insulin.
High-fat low-carb diets are also generally high in nutrient-dense animal foods like meat, eggs, and full-fat dairy. Adding in fresh organ meats, and organ meat supplements will ensure that you’re providing your body the most nutrient-dense foods on earth.
But a ketogenic diet does more than simply cut carbs. When your body runs on fat as fuel, it turns fat into energy molecules called ketones. These compounds have hormone-balancing properties of their own, making them a key factor in the effectiveness of keto diets against insulin resistance.
Insulin Resistance Diet: Takeaway
Diets high in carbohydrates cause your body to produce chronically high levels of insulin in order to move sugar out of your blood and into your cells and liver.
After a while your cells stop responding, the insulin producing cells in your pancreas burn out, and you are left with chronically high levels of blood sugar that can lead to a cascade of diseases and disorders like type 2 diabetes, PCOS, and heart disease among many other.
An insulin resistance diet aims at reversing insulin resistance by changing how we eat.
For decades nutritionists have been recommending a diet high in fibrous fruits and vegetables. Yet these foods are also high in carbohydrates–the root cause of insulin resistance in the first place.
More recently, clinical studies have been showing that high-fat low-carb (ketogenic) diets are far more effective in reducing and reversing insulin resistance.
Additionally, intermittent fasting routines that restrict the time in which you eat are also effective in reducing insulin.
A strong body of research suggests that high-fat low-carb eating and intermittent fasting are likely the most effective approaches when it comes to formulating your insulin resistance diet.